Translate this page into:
Acquired Bartter Like Syndrome in a Patient of Multi Drug Resistant Pulmonary Tuberculosis Secondary to Kanamycin Nephrotoxicity - A Case Report
*See End Note for complete author details
Cite this article as: Bhargude D, Rajadhyaksha A, Vaidya M. Acquired Bartter Like Syndrome in a Patient of Multi Drug Resistant Pulmonary Tuberculosis Secondary to Kanamycin Nephrotoxicity - A Case Report. Global Journal of Medical Students. 2022;2(3):23-7.
Corresponding author: Dr Devesh Bhargude, Department of General Medicine Seth GS Medical College and KEM Hospital. E-mail: devesh.deveshpb.bhargude801@gmail.com
-
Received: ,
Accepted: ,
Abstract
India has the highest estimated burden of tuberculosis infection (TBI) globally caused by Mycobacterium Tuberculosis , with nearly 35-40 crores Indian population having TBI, of which 26 lakhs people (18-36 lakh) are estimated to develop Tuberculosis (TB) disease annually. An integrated and comprehensive ‘cascade of care’ approach and new advances in National Tuberculosis Elimination Program provided us with definitive management of tuberculosis infection and an active tuberculosis disease. Aminoglycosides are one of the cornerstones of drug resistant tuberculosis. Although highly effective they are very notorious for their dose dependent and independent nephrotoxicity . Our experience denotes a rare diagnosis of acquired Bartter like syndrome, in a 60-year man with long standing symp-tomatic pulmonary tuberculosis who received Kanamycin for a period of 5 months and subsequently presented with life threatening elec-trolyte imbalance. Subsequent prognosis showed improvement with conservative treatment and he was discharged in stable condition. It also highlights the importance of adherence to the standard guidelines under National Tuberculosis Elimination Program (NTEP) and the importance of the routine monitoring of electrolytes in Multi-Drug Resistant Tuberculosis (MDR-TB) patients receiving treatment that includes Kanamycin.
Keywords
Bartter syndrome
Aminoglycosides
Kanamycin
Multi-Drug Resistant Pulmonary Tuberculosis
Case Report
INTRODUCTION
Tuberculosis is highly prevalent communicable disease in India. India’s TB incidence for the year 2021 is 210 per 1,00,000 population although declining (256/1,00,000), it carries a significance global average of 11%1 Aminoglycosides remain important drugs in MDR-TB treatment, as they exhibit concentration-dependent bactericidal activity against Mycobacterium tuberculosis and are highly effective in the treatment of drug-resistant TB isolates.2 Estimated number of MDR/RR-TB cases in India are 124 000 (9.1/lakh population). The first NDRS revealed that 28% of TB patients were resistant to any drugs (22% among new and 36.82% among previously treated) and 6.19% had MDR-TB (2.84% among new and 11.62% among PT).3 Aminoglycosides are routinely implied in the treatment of drug resistant tb. Commonly used drugs include Streptomycin, Amikacin, Kanamycin and Capreomycin.4 Kanamycin and Capreomycin, which were associated with poorer outcomes when used and are therefore no longer recommended for use in MDR-TB regimens. Nephrotoxicity induced by aminoglycosides manifests clinically as non-oliguric acute kidney injury, with a slow rise in serum creatinine and a hypo osmolar urinary output developing after several days of treatment.5 Electrolyte disturbances are frequent with aminoglycosides but manifestations in the form of Bartter and Gitelman like syndrome are uncommon. Our case explains the rare occurrence of Bartter like syndrome which is a tubular salt-losing channelopathy in which the kidneys cannot reabsorb sodium and chloride in the thick ascending limb of the loop of Henle in a patient with chronic kanamycin use.6
CASE REPORT
A 60-year-old male, resident of Mumbai, India premorbidly healthy presented to the Emergency Medical Services (EMS) on 18/04/2022 with symptoms of generalised weakness. He was a known case of pulmonary Koch’s diagnosed in view of fever & persistent dry cough 7 months prior to admission. Pulmonary Koch’s was proven radiologically (chest X-ray and high resolution computed tomography of chest) (Figure 1 & 2) but no microbiological evidence. Patient was initiated on anti-tubercular therapy under National tuberculosis elimination program in September 2021. Anti-tubercular therapy consisted of (Tab. Rifampicin 600 mg OD, Tab. Isoniazid 300 mg OD Tab. Ethambutol 1000 mg OD Tab. Pyrazinamide 1250 mg OD). Patient did not improve symptomatically after 2 months of AKT and with a history of multi drug resistant Koch’s contact in his elder daughter he was started on Inj. Kanamycin 750 mg IM every alternate day and Tab. Moxifloxacin 400 mg OD (no confirmatory evidence of MDR Koch’s) empirically by a pulmonologist. Although compliant to treatment, Patient’s symptoms persisted, and he was referred to our hospital for further management.

- HRCT Chest

- Chest X-ray
General examination showed thin built individual with sinus tachycardia, hypotension and was found to be diabetic on admission. Respiratory system examination showed right sided upper lobe crepitations and other system’s examination was within normal limits. Laboratory results on admission revealed severe metabolic alkalosis, hypokalaemia, hyponatraemia, hypocalcaemia, hypomagnesaemia, and hypophosphatemia (Table 1). HIV status came out to be negative. Urine chemistry was suggestive of severe sodium and calcium wasting. After stoppage of Kanamycin injection patient was treated with intravenous fluids, Potassium chloride and Magnesium supplementation. Sputum GeneXpert was suggestive of Multi drug resistant tuberculosis with Rifampicin resistance. Anti-tubercular therapy was switched to Bedaquiline based regimen. Electrolyte monitoring, ECG and daily input-output monitoring was done. Based on reports TTKG (trans tubular potassium gradient) which was >4 suggested distal tubular secretion. In an absence of GI loss and diuretic use, possibility of Gitelman or Bartter like syndrome was raised. To confirm the diagnosis urine calcium/urine creatinine ratio was calculated which was >0.20 confirming hypercalciuria and thus the diagnosis of acquired Bartter like syndrome (Table 2) was confirmed. Patient was treated conservatively with normal saline and potassium supplementation and was discharged in vitally stable condition.
| Date/parameters | Day 1 | Day 3 | Day 6 | Day 9 |
|---|---|---|---|---|
| Bun | 8 | 5 | 6 | |
| creatinine | 1.3 | 1.1 | 1.2 | |
| Sodium | 130 | 136 | 129 | 133 |
| Potassium | 2.1 | 2.6 | 4.5 | 4.9 |
| Chloride | 97 | 99 | ||
| Hb | 7.4 | 7 | 8 | 10.9 |
| TLC | 5800 | 3500 | 1.0l | 2.0l |
| Platelets | 1.6l | 1.2l | 12l | 2.0l |
| SGOT | 30 | 30 | 30 | 32 |
| SGPT | 10 | 10 | 10 | 18 |
| Parameters | Value | Normal Range |
Depending on diet(mg/ day) |
Day 9 |
|---|---|---|---|---|
| Urine electrolytes(mg/ day) |
In (mg/ day ) |
8 | 5 | 6 |
| Sodium (meq/ day) |
105.6 | 40-220 | 1.1 | 1.2 |
| Potassium (meq/ day) |
32.1 | 40-80 | 129 | 133 |
| Chloride (meq/ day) |
118 | 110-250 | 4.5 | 4.9 |
| Urine (mg/dl) creatinine | 14.7 (mg/ dl) |
20-275 (mg/dl) |
99 | |
| Serum osmolality (mosm/kg) | 276 | 275-300 | 8 | 10.9 |
| Urine osmolality (mosm/kg) |
380 | 50-1200 | 1.0l | 2.0l |
| Urine calcium (mmol) | 8.6 | 2.50-7.50 | 10 | 18 |
DISCUSSION
Aminoglycosides are well known for their nephrotoxicity and commonly cause acute tubular necrosis, manifesting as Fanconi syndrome, distal renal tubular acidosis and uncommonly as Bartter-like syndrome7 and Gitelman like syndrome. Aminoglycosides that have been implicated in causing this syndrome include Gentamicin,8 Amikacin,9 Tobramycin8 and Netilmicin10 and Kanamycin. The most nephrotoxic is Neomycin followed by Gentamicin, least nephrotoxic Streptomycin.11 Kanamycin has intermediate toxicity. This variability is partly related to the cationic charge that is generated by the number of amine groups attached to the drug.
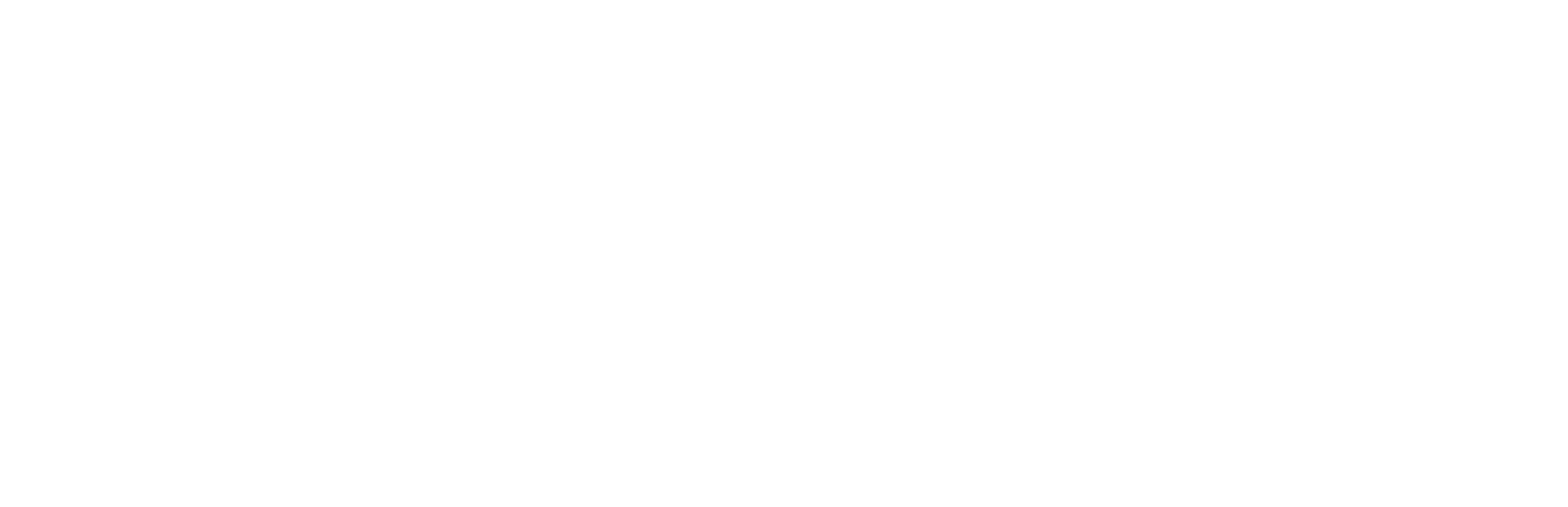
Bartter syndrome is a renal disease characterized by an inability of the thick ascending limb of the loop of Henle (TALH) to reabsorb salt and was first described by Dr F. Bartter in 1962.12 Bartter syndrome may be inherited or acquired. In the case of aminoglycosides, it is thought to be a result of stimulation of the calcium-sensing receptor (CaSR) (black block in Figure 3) that is located on the basolateral surface of principal cells lining the thick ascending limb of the loop of Henle.13
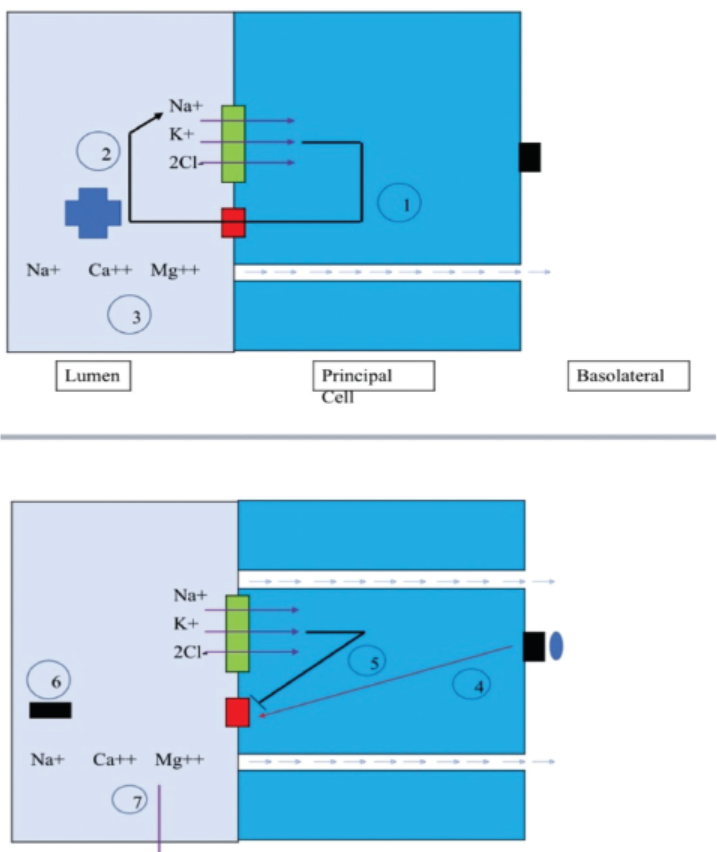
- Pathogenesis of Bartter syndrome
The CaSR is a cell surface receptor with unique property such that it does not have a single but can be stimulated by numerous polyvalent cationic compounds, including aminoglycoside antibiotics. Stimulation of this receptor closes the rat outer medulla potassium (ROMK) channel (red square in Figure 3) located at the luminal surface, preventing potassium recycling. This has two effects: (1) the sodium-potassium-2 chloride cotransporter (NKCC) (green rectangle Figure 3) ceases to function, and (2) loss of the lumen-positive charge prevents the normal paracellular reabsorption of sodium, magnesium, and calcium (Figure 3).14
CONCLUSION
Our experience highlights the importance of guideline-based therapy.
Owing to the property of saturation, aminoglycosides should be used as a daily single dosage.
Importance of electrolyte monitoring for Aminoglycoside recipients.
END NOTE
Author Information
-
Dr Devesh Bhargude
Department of General Medicine, Seth GS Medical College and KEM Hospital
Dr. Anjali Rajadhyaksha, Professor, Department of General Medicine, Seth GS and KEM Hospital
Dr. Meghna Vaidya, Associate Professor, Department of General Medicine, Seth GS and KEM Hospital
Conflict of Interest:
None declared
Abbreviations:
OD - once daily
Tab - tablet
MDR - multi drug resistant
REFERENCES
- Successful MDR-TB treatment regimens including amikacin are associated with high rates of hearing loss. BMC Infect Dis. 2014;14:542.
- [CrossRef] [PubMed] [Google Scholar]
- Guidelnes for programmatic management of drug resistant tubercu-losis in India. 2021 MARCH:6.
- [Google Scholar]
- Guidelnes for programmatic management of drug resistant tubercu-losis in India. 2021 MARCH:42.
- [Google Scholar]
- Aminoglycosides: nephrotoxicity. Antimicrob Agents Chemother. 1999;43(5):1003-12.
- [CrossRef] [PubMed] [Google Scholar]
- Bartter Syndrome. In: StatPearls [Internet] Treasure Island (FL): StatPearls Publishing; 2022.
- [Google Scholar]
- Aminoglycoside-induced nephrotoxicity. J Pharm Pract. 2014;27:573-577.
- [CrossRef] [PubMed] [Google Scholar]
- The Case - Metabolic alka-losis in a patient with cystic fibrosis. Kidney Int. 2012;81(4):421-2.
- [CrossRef] [PubMed] [Google Scholar]
- Amikacin-induced type 5 Bartter-like syndrome with severe hypocalcemia.} Postgrad Med. 2009;55:208.
- [CrossRef] [PubMed] [Google Scholar]
- Acquired Bartter-like syndrome associa-tion with netilmicin therapy in an extremely low birth weight infant. Ren Fail. 2014;36(1):123-5.
- [CrossRef] [PubMed] [Google Scholar]
- Gitelman-like Syn-drome with Kanamycin Toxicity. J Assoc Physicians India. 2016;64(5):90-2.
- [Google Scholar]
- Aminoglycoside antibiotics induce pH-sensitive activation of the calcium-sensing receptor. Biochem Biophys Res Commun. 2002;297(1):71-7.
- [CrossRef] [PubMed] [Google Scholar]
- Bartter-like syndrome caused by kanamycin during therapy for multidrug-resistant Myco-bacterium tuberculosis. African Journal of Nephrology. 2018;21(1):16-9.
- [CrossRef] [Google Scholar]