Environment-Friendly and Sustainable Oncological Care Settings in the Times of COVID-19: A Narrative Review
Corresponding author: Dr. Suvam Banerjee 2/3, Dewangazi Road, Bally, Howrah-711201, West Bengal, India. E-mail address: banerjeesuvam1@gmail.com
-
Received: ,
Accepted: ,
Abstract
The increased use of personal protective equipment (PPE) has become a necessity for successful protection against SARS-CoV-2 both to medical personnel and patients. The varied examples include disposable masks, eye goggles, gloves and other such equipment. While having its positive aspects, using PPE has also been known to cause delirious effects on the environment due to its low level of safety, utility and recyclability. This review aims to address the importance of finding an alternative to the currently used PPE. The specific targets of this review focus on equipment used in oncological administrations. The literature review was conducted using various databases and based on selected inclusion and exclusion criteria, articles were assessed independently by 2 scientific reviewers. Evidence from included papers states that there has been a heightened demand for reusing PPE. There is evidence for offering various strategies for more successful production and reusing of PPE. This analysis and collective evidence would aid in bringing an advanced understanding for the development of more ecologically-friendly equipment options in oncology.
Keywords
COVID-19
Oncology
Ecofriendly
Sustainability
Review
INTRODUCTION
The coronavirus disease 2019 (COVID-19) has posed a real challenge for oncological settings. In this context, oncological patients are at great risk of infection due to immunosuppression associated with the treatment. Appropriate use of specific and personal protective equipment (PPE) in such settings is essential to reduce the chance of contracting severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. However, given the emergence of new variants of SARS-CoV-2 in the face of the long duration of the pandemic,1-3 there is an imminent need to develop new methodologies for a sustainable and safe oncological approach for patients and healthcare professionals. From an environmental point of view, the carbon impression must be taken seriously for there to be an effective success in the combination of cancer treatment and PPE.
Environment-friendly clinical setups to deliver eco-friendly oncological health care are of paramount importance in modern times, especially during the COVID-19 pandemic. Cancer, including solid tumours and haematological malignancies, still accounts for the second leading cause of mortality all over the world and is estimated to be responsible for 9.6 million annual deaths globally in 2018.3-5 Cancer patients are highly vulnerable to contracting the virus and suffer from serious morbidities associated with COVID-19. They receive different modalities of anti-cancer treatment and supportive therapies (for example, immunosuppressive drugs like steroids etc.) regularly which might make them immuno-compromised. Malignancies also have an immunosuppressive action on their own. Moreover, cancer in the elderly population makes them highly susceptible towards COVID-19-related complications and mortality due to their comorbidities such as diabetes, hypertension etc. Studies have reported how acquiring the COVID-19 disease along with several other risk factors has a positive association with 30 days of all-cause mortality in the cancer-affected population.1,6
Eco-environmental factors which lead to the transmission of coronavirus disease and its dreadful impact on cancer patients must be understood. Transmission of the virus is also caused by several environmental sources other than direct transmission which includes hospital wastes, air aerosols, public use wastes, municipal wastes, ventilation facilities, soil and groundwater etc.6-8 Although the lockdowns during the pandemic have decreased the rate of noise and air pollution, increased use of gloves and masks as part of personal protective equipment (PPE), especially in hospital settings have posed a serious threat to the environment by increasing the carbon impression globally. However, the usage of this equipment has also become very essential in oncological healthcare setups to prevent transmission of the virus and hence protect cancer patients from its associated morbidities and mortalities. Thus, setting up environment friendly and sustainable oncological care settings during the times of the pandemic has become a need of the hour.
The pandemic has posed a real threat to the different modalities of cancer management- prevention, diagnosis and treatment. With the rise of new cases every year all around the globe, it has become very essential to ensure the proper management of cancer patients, especially during the times of COVID-19. This has a profound impact on the entire oncology community by affecting both the cancer patients as well as the caregivers. There has been an urgent necessity to propose and promote several modifications in oncological care settings especially the hospital wards to protect the patients and caregivers from the coronavirus infection, while simultaneously maintaining cancer diagnosis, treatment, and research.8 There are higher risks of contamination of the healthcare providers which may profoundly challenge the healthcare systems globally. Due to compromised immune systems in cancer patients, they become extremely susceptible to several infections by various types of pathogens (bacterial, viral and fungal) and thus environment-friendly approaches to prevent transmission of infections become highly relevant in clinics during the pandemic as COVID-19 has been associated with increased mortality.8,9 While there may be debate as to whether it is a rational approach to look at the consequences of cancer at the time of COVID-19 especially when its incidence is at its peak, it should also be noted that we need to prioritize the mid-term and long-term impacts on cancer to prevent its associated complications during and after the pandemic ends.
The purpose of the review is to investigate whether there is a possibility to find new alternatives to existing PPEs at an oncological level of care. The discussion in this review includes the necessity to find alternative reusable PPE primarily in the medical environment. It is deemed necessary to weigh the importance of SARS-CoV-2 on social, economic and environmental aspects.
METHODS & RESULTS
The reporting of this narrative review was based on the Scale for the Assessment of Narrative Review Articles (SANRA).10 A literature search was performed in four databases, namely PubMed, EBSCOhost, ScienceDirect and Scopus. Papers were searched through databases using the following keywords: “carbon emission” AND “environment” AND “COVID-19”. After searching for papers, duplicates were removed and articles which contained requested keywords in the title or abstract and corresponded to specified search criteria were processed for further examination.
Articles were included if they (1) consisted of an extensive literature search as a systematic literature review or meta-analysis, and (2) focused on discussing the ecologically-friendly ways of PPE during the global pandemic in oncology settings. Exclusion criterium for articles was: (1) if articles focused on the general usability of PPE in the medical environment during the pandemic and (2) if articles discussed the influence of vaccines or COVID-19 on people’s health. Only articles in English were included in this review.
Results showed 164 articles from PubMed, 76 from EBSCOhost, 145 from Scopus and 4579 from Science Direct. After reducing 4933 duplicates and after the full-text screening, 31 papers were included in this review.
DISCUSSION
The influence of COVID-19 on global healthcare
To further discuss the importance of COVID-19 on global health, it is necessary to state how the virus can be transmitted. Face-to-face transmission is executed by respiratory droplets and infected secretions such as saliva, and further distance transmission is possible through airborne droplet nuclei. Moreover, the virus can remain viable for some time on different surfaces (e.g., it stays viable for 3 hours on paper, 7 days on plastic, etc.).11,12 There is no evidence that COVID-19 can be spread via blood contact or transfusion. It is quite hard to track infection rates of COVID-19 as cumulative coefficients of new cases are different per country and at some times of the year, rates were higher. Additionally, the precise number of COVID-19 cases remains unknown, which makes calculations even harder.13-15
The global pandemic caused by SARS-CoV-2 has led to numerous changes in ordinary lives. People had to stay mostly at their homes and minimize social contact with their friends or beloved ones, events got cancelled, a new stressful environment was introduced to humanity and other lockdown complications. From a positive perspective, after the most severe COVID-19 outbreaks healthcare systems started encouraging people to take more concern about their health and hygiene, and also follow recommendations for maintaining a healthy lifestyle, increasing education about pathogens and the ways how to oppose them. On the other hand, there is no doubt that the biggest advantage of the COVID-19 pandemic was showing that global healthcare is not ready yet to oppose the fast transmission of disease, even though humanity has already witnessed many pandemics throughout history.12,13,16,17
Several drawbacks of current global healthcare could be mentioned. Numerous countries have implemented late quarantine rules and restrictions which led to poor consequences (for example, the United Kingdom). Not enough money is spent on healthcare in countries; thus, it makes it harder for developing countries to withstand disease and provide full medical support for COVID-19-positive people. Additionally, high medical care costs made it problematic for poorer people to reach medical support even in developed countries. Little investments were put into mental care, as stress and isolated lives increased depression and anxiety in the population. Research on treatment and vaccine development has been relatively fast compared to all previous vaccines development, yet it was not fast enough to save many people’s lives, not to mention that the production of vaccines raises important environmental concerns.18
Oncological setups during COVID-19 outbreak
The pandemic has imposed a serious challenge to healthcare settings globally. Oncological care settings have faced an unprecedented threat as cancer patients are more likely to have lower levels of immunity and hence require a multidisciplinary treatment approach. Hospital beds have been scarce, decreased supply of medications including life-saving drugs as well as a crisis in healthcare providers including nurses, physicians and health staff. To cope with these crises effectively, there has been a transformation in strategies to promote effective cancer management in oncological setups globally including hospital wards or indoors as well as in outpatient management and clinics.19,20 This shall continue with minimal resources over a short period and the role of telemedicine in oncological care is gradually evolving in virtual consultations.
The transformation in the delivery of oncological care includes consultations, systemic therapy against cancer, and surgery for patients while preventing them from contracting the virus and other infections effectively. It has been reported that as a result of this transformation or personal choice of the patients, there was a 30% reduction of patients receiving anti-cancer treatment like chemotherapy on an average and up to 50% decline in new cases presenting or have been referred for diagnosis of suspected cancer in March to April 2020.19 However, emergency cancer care continued, whereas the rest including referrals started to be conducted virtually. To prevent transmission of the virus and other pathogens, safety strategies have been proposed to ensure the compulsory wearing of PPE (personal protective equipment) by patients and caregivers as well as promoting home delivery of some systemic anti-cancer medicines such as Herceptin, administered by subcutaneous route or Tyrosine Kinase inhibitors etc. These enable social distancing and prevent unnecessary hospital visits and save time, making it convenient for both cancer patients as well as healthcare providers.19-21 In many centres, only those procedures or examinations which were instrumental, clinical and targeted were performed. Separate inpatient units and daycare setups for COVID-19-positive and negative patients have been built to prevent the transmission of infections. Self-isolation has been recommended for COVID-positive or symptomatic staff or patients and a negative swab test was required to return to work in most of the centres.21
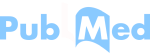
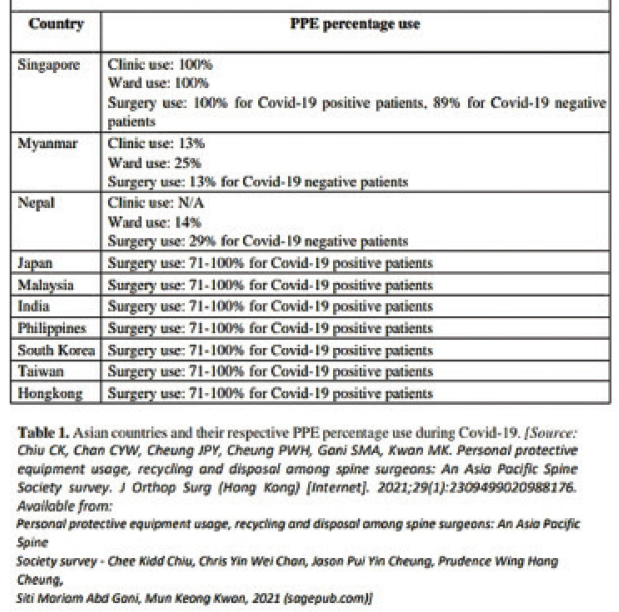
The usage of personal protective equipment (PPE) has been considered to be the most effective strategy to protect patients and caregivers in cancer clinics against the virus by limiting its transmission (Table – 1) and (Table – 2). It has been the need of the hour to set up a rational approach regarding the usage of PPE effectively in operative settings of cancer management, in cases of COVID-19 positive as well as negative patients. PPEs should be of great help in providing optimum levels of cancer care and reducing the negative effects of any delays in cancer treatment including surgeries. The N95 masks along with 3-ply masks, respirator masks, disposable or reusable gowns, face shields and goggles, wearing double gloves, regular power glasses etc. are integral components of the PPE. It has been reported that N-95 masks/double gloves or gowns (disposable/ reusable) and eye protection devices with or without shoe covers were the most common PPE combination used by cancer surgeons while performing several operations during the pandemic.20-22 However, there have been complaints of severe stress and discomfort associated with the usage of PPEs by healthcare workers especially for prolonged periods. There have been reports of contact dermatitis, headache, fatigue, difficulty in communication and breathing problems with poor vision, fogging, and irritation of the skin with the usage of different components of PPE.20 The N-95 masks and eye protection component has been attributed with causing maximum discomfort to cancer surgeons. This is aggravated by the presence of pre-existing health illnesses like asthma, migraine, claustrophobia etc. Studies have reported the beneficial impact of minimally invasive surgeries during the pandemic wherever applicable in cancer patients.21,23 There have been strong recommendations for using laparoscopy during the pandemic.
 |
 |
The National Institute for Health and Care Excellence (NICE) has framed a triage system to classify cancer patients by their chances of survival from therapy. This system would be beneficial in guiding physicians to make better decisions considering different clinical aspects of cancer care. Patients who require surgeries or other procedures to be performed can be referred to the newly built cancer centres which have been made COVID-free. A prioritization system has been set up for their surgeries.22,24,25 According to this, four types of priorities should be considered as follows:
Priority 1a: Emergency operation- surgery when needed to save a life, to be performed within 24 hours.
Priority 1b: Urgent operation- surgery required within 72 hours.
Priority 2: Elective operation- surgery required to be performed within 4 weeks as a life-saving procedure or to prevent disease progression.
Priority 3: Elective operation- there can be a delay in surgery for up to 10-12 weeks without any prediction of the negative outcome.
Though emergency surgical procedures are being continued to be performed, there is concern regarding elective or planned surgeries in cancer patients. There is a huge concern regarding the postponement of elective surgeries in patients especially with solid tumours because this might lead to disease progression due to delays in operation. This also needs to be balanced against the risk of exposing susceptible individuals to the virus. Studies have reported that by following standard precautionary measures recommended by PHE and RCS however, elective surgeries can be performed safely in cancer patients during the pandemic in acute hospitals.26 There is also a positive finding the patients who did not have increased rates of infection from COVID-19 were admitted post-operatively. Proper screening of patients should be encouraged and proper infrastructure for testing should be developed for this purpose. RCS has recommended that before elective operations, patients must be asymptomatic and should have self-isolated for two weeks and have an RT-PCR test for COVID-19 negative. It has also been recommended for periodic testing of all healthcare providers to reduce transmission of infections.
A study by COVIDSurg Collaborative, as a part of a project by The University of Birmingham and the National Institute for Health Research (NIHR), has reported the fragility in oncological surgery systems globally during lockdowns.27,28
This is an international, pan-speciality project with a multicentric approach to evaluate several end-points, including 30-day mortality in COVID-19 patients, the impact on safety in operations in cancer setups and its effect on unnecessary delays, as well as its effect on the surgical team and emergency operations. According to this study, every one in seven cancer patients, as residents of regions with full lockdowns, did not undergo elective surgeries and experienced longer delays during their preoperative period. These could lead to reductions in their survival rates as long-term impact. This has suggested that the planned surgeries require strengthening of their infrastructure which includes protected planned operative procedures and long-term investment for critical care in surge capacities to protect the healthcare providers and services during public health emergencies in the future like this pandemic. It has also provided key areas of transforming the practices for safe surgical management globally during the pandemic, as follows:29
Framing a proper scientific plan to promote surgeries worldwide which includes postponement of planned surgeries, repurposing rooms for operations (OR) as areas of critical management of patients and surgical workflow.
Forming a team approach for promoting emergency operations during COVID-19.
Providing health education to healthcare workers on PPE usage and management of COVID-19 to promote safe operations during the times of pandemic.
Screening and management of COVID-19 infections while preventing exposure of healthcare providers. E. Build a dedicated space for surgeries during the pandemic as a part of a wider clinical response.
The safe disposal of surgical wastes including post-operative specimens in cases of cancer surgeries is a real challenge during the pandemic. They should be labelled as “COVID-19 suspected” and sealed in the operating rooms (ORs) along with all other human anatomical wastes, body fluids, disposable materials, PPE and gowns (double-bagged), tubings etc. They should have a label on them with a sign implying it is from an OR with either a suspected or confirmed COVID-19 patient and should be safely disposed of following the local guidelines for infectious waste management.29-31 Following this, the OR must have proper disinfection and sterilization, including anaesthetic equipment and operating table, with a chlorine-based disinfectant or alcohol (minimum of 75%). This will prevent the virus from surviving on hightouch surfaces for a long period.
CONCLUSION
The ecological effect of PPE is significant and requires an earnest audit, particularly in oncology care settings to relieve impacts on planetary wellbeing. The most perfect and significant systems might be through decreased utilization of gloves by utilizing hand washing alone, homegrown production of PPE, and expanded use or reuse of PPE like veils and outfits. These prospects warrant further examination and investigation of attainability and well-being, just as the commitment of strategy creators all over the planet.
END NOTE
Author Information
Suvam Banerjee, House Physician, Burdwan Medical College and Hospital, West Bengal, India
Elina Semenenko, Clinical neuro-psychologist, Faculty of Psychology and Neuroscience, Maastricht University, Maastricht, Netherlands.
Conflict of Interest
None declared
References
- Emergence of SARSCoV-2 New Variants and Their Clinical Significance. Canadian Journal of Infectious Diseases and Medical Microbiology. 2022;2022:7336309.
- [CrossRef] [Google Scholar]
- COVID-19 and Cancer Consortium. Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. Lancet. 2020;395(10241):1907-1918. Epub 2020 May 28
- [CrossRef] [Google Scholar]
- Eco-Environmental Aspects of COVID-19 Pandemic and Potential Control Strategies. Int J Environ Res Public Health. 2021;18(7):3488.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Impact of the COVID-19 Outbreak on the Management of Patients with Cancer. Target Oncol. 2020;15(3):249-259.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- COVID-19 in cancer patients: update from the joint analysis of the ESMO-CoCARE, BSMO, and PSMO international databases. ESMO Open. 2023;8(3):101566. Epub ahead of print
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Severe SARS-CoV-2 infection as a marker of undiagnosed cancer: a population-based study. Sci Rep. 2023;13(1):8729.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Fighting against the common enemy of COVID-19: a practice of building a community with a shared future for mankind. Infect Dis Poverty. 2020;9(1):34.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Virology, Epidemiology, Pathogenesis, and Control of COVID-19. Viruses. 2020;12(4):372.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Coronavirus Pandemic (COVID-19) 2020. [Internet]. Available from: Coronavirus Pandemic (COVID-19) - Our World in Data
- [Google Scholar]
- SANRA-a scale for the quality assessment of narrative review articles. Res Integr Peer Rev. 2019;4:5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science [Internet]. 2020;367(6483):1260-1263. Available from: Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation | Science doi:
- [CrossRef] [Google Scholar]
- NIH: National Institute of Allergy and Infectious Diseases. 2019. [Internet]. Available from: https://www.niaid.nih.gov/research/vaccine-types
- [Google Scholar]
- COVID-19 vaccine: what are we doing and what should we do? The Lancet [Internet]. 2022;22(5):569-570. Available from: COVID-19 vaccine: what are we doing and what should we do?-The Lancet Infectious Diseases doi:
- [CrossRef] [Google Scholar]
- 2022. [Internet]. Available from: Coronavirus disease (COVID-19): Vaccines (who.int)
- Stability of SARS-CoV-2 in different environmental conditions. The Lancet Microbe [Internet] . 2022;1(1):E10.
- [CrossRef] [Google Scholar]
- A simple mathematical tool to forecast COVID-19 cumulative case numbers. Clin Epidemiol Glob Health. 2021;12:100853.
- [CrossRef] [Google Scholar]
- Health inequalities and infectious disease epidemics: a challenge for global health security. Biosecur Bioterror. 2014;12(5):263-273.
- [CrossRef] [Google Scholar]
- Role of technology in COVID-19 pandemic. Researches and Applications of Artificial Intelligence to Mitigate Pandemics [Internet] 2021:109-138.
- [CrossRef] [Google Scholar]
- COVID-19 and Oncology: Service transformation during pandemic. Cancer Med. 2020;9(19):7161-7171. Epub 2020 Aug 18
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Pharmacological Prophylaxis and Personal Protective Equipment (PPE) Practices in Gynecological Cancer Surgery During COVID-19 Pandemic. Indian J Gynecol Oncol. 2021;19(1):19. Epub 2021 Jan 30
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A Survey of Personnel Protective equipment’s (PPE) Use and Comfort Levels Among Surgeons During Routine Cancer Surgery in the COVID-19 Pandemic. Indian J Surg Oncol. 2021;12(2):365-373. Epub 2021 Mar 26
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- International guidelines and recommendations for surgery during Covid-19 pandemic: A Systematic Review. Int J Surg. 2020;79:180-188. Epub 2020 May 23
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Effect of COVID-19 pandemic lock-downs on planned cancer surgery for 15 tumour types in 61 countries: an international, prospective, cohort study. Lancet Oncol. 2021;22(11):1507-1517. Epub 2021 Oct 5
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Impact of the Corona-virus (COVID-19) pandemic on surgical practice–Part 1. Int J Surg. 2020;79:168-179. Epub 2020 May 12
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Learning opportunities from COVID-19 and future effects on health care system. Diabetes Metab Syndr. 2020;14(5):943-946. Epub 2020 Jun 20
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Headaches Associated With Personal Protective Equipment–A Cross-Sectional Study Among Frontline Healthcare Workers During COVID-19. Headache. 2020;60(5):864-877. Epub 2020 Apr 12
- [CrossRef] [PubMed] [Google Scholar]
- Impact of Personal Protective Equipment on Surgical Performance During the COVID-19 Pandemic. World J Surg. 2020;44(9):2842-2847.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Emergency and essential surgical healthcare services during COVID-19 in low-and middle-income countries: A perspective. Int J Surg. 2020;79:43-46.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Elective Cancer Surgery in COVID-19-Free Surgical Pathways During the SARS-CoV-2 Pandemic: An International, Multicenter, Comparative Cohort Study. J Clin Oncol. 2021;39(1):66-78.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A commentary on “Impact of the Coronavirus (COVID-19) pandemic on surgical practice–Part 1”. Int J Surg. 2020;82:200-201.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- COVID-19 Creating another problem? Sustainable solution for PPE disposal through LCA approach. Environ Dev Sustain [Internet]. 2021;23(6):9418-9432. Available from: COVID-19 Creating another problem? Sustainable solution for PPE disposal through LCA approach-PMC (nih.gov) doi:
- [CrossRef] [Google Scholar]